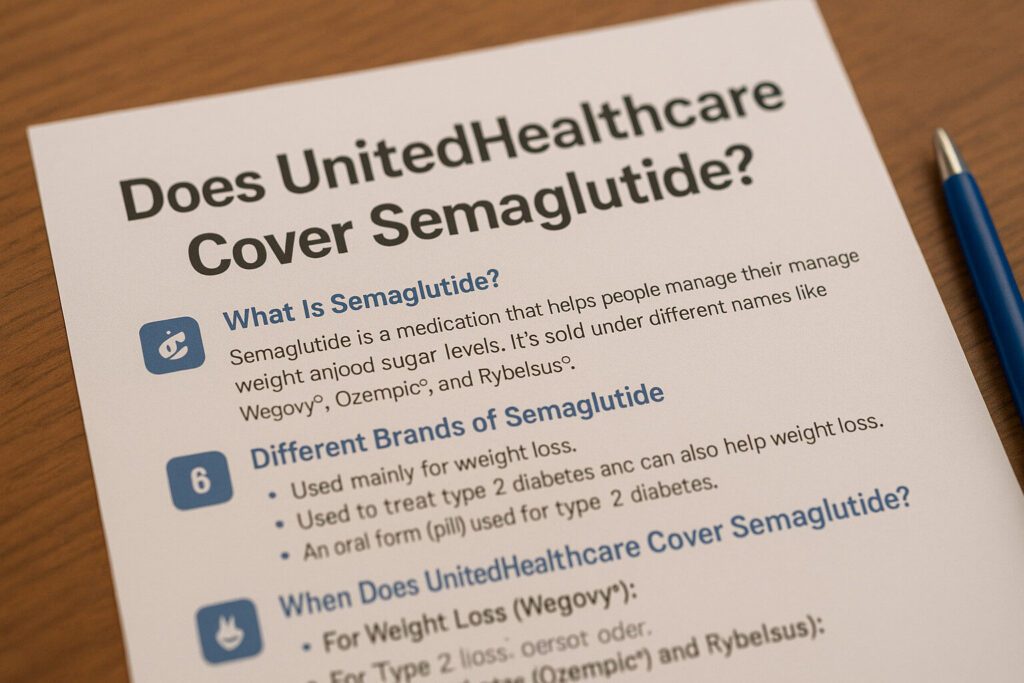
Does United Healthcare Cover Semaglutide?
Semaglutide is a medication that helps people manage their weight and control blood sugar levels. It’s sold under different names like Wegovy®, Ozempic®, and Rybelsus®. United Healthcare (UHC) may cover semaglutide, but it depends on your specific health plan and medical needs.
What Is Semaglutide?
Semaglutide is a medicine that helps people lose weight and manage type 2 diabetes. It works by mimicking a hormone in your body that controls appetite and blood sugar. This means you feel full sooner and eat less, which can lead to weight loss and better blood sugar control.
💊 Different Brands of Semaglutide
- Wegovy®: Used mainly for weight loss.
- Ozempic®: Used to treat type 2 diabetes and can also help with weight loss.
- Rybelsus®: An oral form (pill) used for type 2 diabetes.
✅ When Does UnitedHealthcare Cover Semaglutide?
United Healthcare may cover semaglutide if you meet certain conditions:Allergy Care & Weight Loss | Curex
- For Weight Loss (Wegovy®):
- You are 18 years or older.
- Your Body Mass Index (BMI) is 30 or higher, or 27 or higher with a weight-related health problem like high blood pressure or type 2 diabetes.
- You’ve tried to lose weight through diet and exercise without success.
- You’re enrolled in a weight management program.
- For Type 2 Diabetes (Ozempic® and Rybelsus®):
- You have a diagnosis of type 2 diabetes.
- Other diabetes medications haven’t worked well for you.
Coverage often requires prior authorization, meaning your doctor must get approval from UHC before you can get the medication.
Understanding Semaglutide and Its Uses
Semaglutide is a medication that mimics a natural hormone in the body to regulate appetite and blood sugar levels. It’s available under different brand names:
- Wegovy®: Primarily prescribed for weight management in individuals with obesity or overweight conditions.
- Ozempic®: Used to manage type 2 diabetes and can also aid in weight loss.
- Rybelsus®: An oral form of semaglutide for type 2 diabetes management.
Why Might Coverage Be Denied?
United Healthcare might not cover semaglutide if:Allergy Care & Weight Loss | Curex+2Allergy Care & Weight Loss | Curex+2Allergy Care & Weight Loss | Curex+2
- You don’t meet the BMI or health condition requirements.
- You haven’t tried other treatments first.
- You’re not enrolled in a weight management program.
- The medication is prescribed for a use not approved by UHC.
Even if you meet the criteria, coverage can vary based on your specific health plan.
💵 How Much Does Semaglutide Cost Without Insurance?
If you don’t have insurance coverage, semaglutide can be expensive:
- Wegovy®: Around $1,200 to $1,400 per month.
- Ozempic®: Similar cost range.
- Rybelsus®: Costs can vary.Reuters+2NowPatient+2UnitedHealthcare+2
These prices can be a burden, so it’s important to check if your insurance covers the medication.
📝 How to Check If You’re Covered
- Review Your Plan: Look at your United Healthcare plan documents or online portal to see if semaglutide is covered.
- Talk to Your Doctor: They can help determine if you meet the criteria and assist with the prior authorization process.
- Contact UHC: Call the number on your insurance card to ask about coverage for semaglutide.
📄 What If Coverage Is Denied?
If United Healthcare denies coverage:
- Appeal the Decision: You can file an appeal with UHC. Your doctor can help provide additional information to support your case.
- Explore Alternatives: Ask your doctor about other medications or treatments that might be covered.
- Check for Assistance Programs: Some pharmaceutical companies offer programs to help reduce the cost of medications.
UnitedHealthcare’s Coverage Criteria for Semaglutide
1. Coverage for Wegovy® (Weight Management)
UHC may cover Wegovy® under specific conditions:
- Body Mass Index (BMI):
- Adults with a BMI of 30 kg/m² or higher.
- Adults with a BMI of 27 kg/m² or higher accompanied by at least one weight-related health condition (e.g., hypertension, type 2 diabetes, or high cholesterol).
- Age Requirement: Individuals aged 18 years or older.
- Lifestyle Modification: Participation in a weight management program that includes diet, exercise, and behavioral changes.
- Medical Supervision: Prescription and ongoing monitoring by a healthcare provider specializing in weight management.
- Documentation: Evidence of previous unsuccessful weight loss attempts through lifestyle changes alone.
For continued coverage beyond the initial period, UHC typically requires:
- Demonstrated Weight Loss: At least 5% reduction in body weight from the start of treatment.
- Ongoing Lifestyle Efforts: Continued adherence to diet, exercise, and behavioral strategies.
Source: UHC Provider – Weight Loss Medication Coverage
2. Coverage for Ozempic® and Rybelsus® (Type 2 Diabetes Management)
UHC’s coverage for these medications generally includes:
- Diagnosis: Confirmed type 2 diabetes.
- Previous Treatments: Inadequate blood sugar control with other medications like metformin.
- Medical Necessity: Documentation supporting the need for semaglutide based on medical evaluations.
- Prior Authorization: Approval from UHC before starting the medication, often requiring detailed medical records.
Note: While Ozempic® may lead to weight loss, UHC typically does not cover it solely for weight management purposes.
Source: SingleCare – Does UnitedHealthcare Cover Ozempic?
Navigating Prior Authorization with UHC
Prior Authorization (PA) is a process where UHC reviews and approves certain medications before coverage is granted. To navigate this:
- Consult Your Healthcare Provider: Discuss the need for semaglutide and ensure they are prepared to provide necessary documentation.
- Gather Documentation: This includes medical history, previous treatment attempts, and current health status.
- Submit PA Request: Your provider will send the request to UHC, including all supporting documents.
- Follow Up: Stay in contact with both your provider and UHC to monitor the status of the request.
- Appeal if Denied: If coverage is denied, you have the right to appeal the decision with additional information or clarification.


